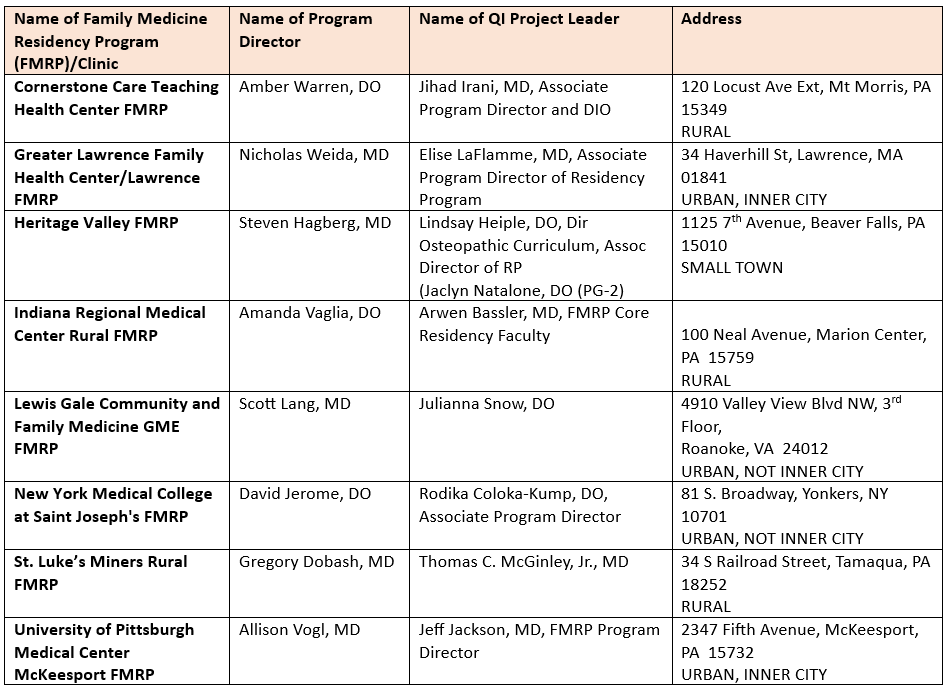
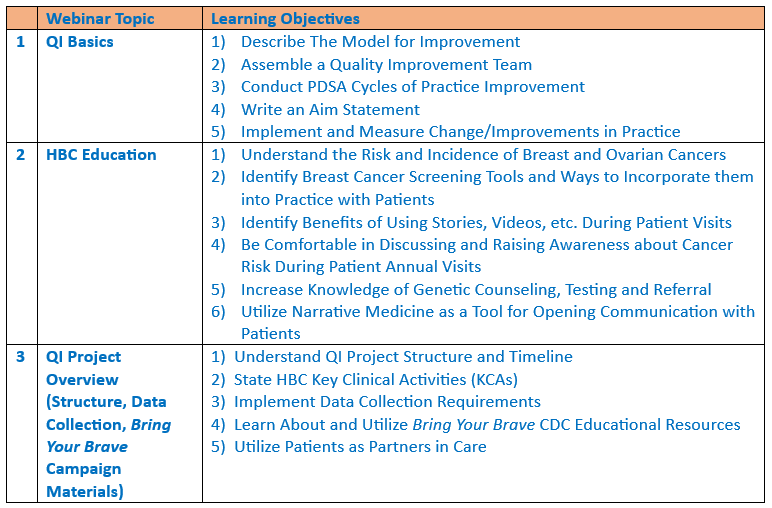
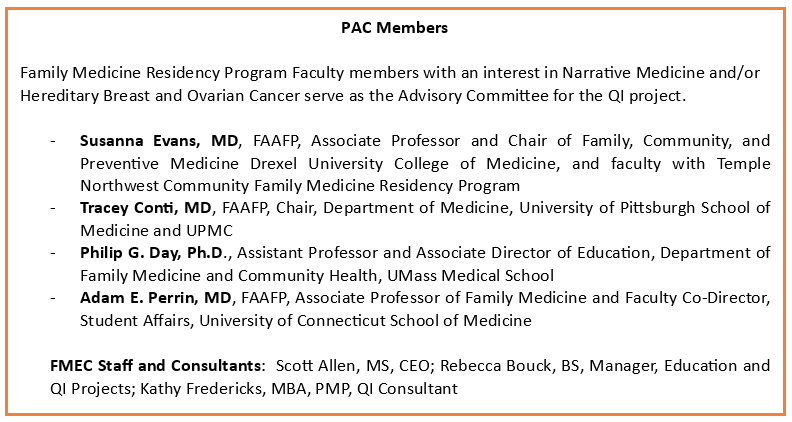
Hereditary Breast Cancer Quality Improvement Pilot ProjectFrom 2023-2024, the Family Medicine Education Consortium (FMEC) partnered with the National Association of Chronic Disease Directors on a cancer prevention and early detection quality improvement (QI) pilot project funded by the Centers for Disease Control and Prevention (CDC). As of July 2024 The results shown by the end of the collaborative are impressive for the short period measured. Cancer screening rates, discussing screening findings with patients, sharing CDC Bring Your Brave (BYB) patient education resources, and referring patients who screened positive for genetic counseling or testing had greatly improved among the participating FMRPs. Participants reported being meaningfully involved in the pilot including learning about and executing the project, reviewing data in keeping with the project’s measurement plan, being involved in changes implemented during the project, and participating in meetings or conversations about the project. When asked whether participants intended to continue to assess patients for risk of hereditary breast or ovarian cancer at the conclusion of the pilot, 96% responded yes. When asked whether participants think they will continue to offer the BYB resources to patients who screen positive, 92% responded yes. QI leaders expressed a high degree of satisfaction with the project and would recommend this type of a QI activity to their colleagues. CDC, FMEC, and NACDD have received many heartfelt and thoughtful comments from family physicians about the impact of the BYB materials. All of the FMRPs involved with this pilot are sharing CDC BYB educational resources with patients who screen positive for HBC. Participants Family Medicine Residency Program Participants Access the Training Recordings and PDFs of Slide Presentations Hereditary Breast Cancer Education and Bring Your Brave CDC Educational Resources, January 17, 2024 Quality Improvement Basics, January 25, 2024 Project Structure, Timeline, and Data Collection Requirements, February 1, 2024 CME and Performance Improvement Credits The AAFP has reviewed Family Medicine Education Consortium (FMEC) Hereditary Breast Cancer Quality Improvement Pilot Project and deemed it acceptable for up to 20.00 Performance Improvement AAFP Prescribed credits. Term of Approval is from 12/01/2023 to 07/31/2024. Physicians should claim only the credit commensurate with the extent of their participation in the activity. AAFP Prescribed credit is accepted by the American Medical Association as equivalent to AMA PRA Category 1 credit(s)™ toward the AMA Physician's Recognition Award. When applying for the AMA PRA, Prescribed credit earned must be reported as Prescribed, not as Category 1. Acknowledgements HBC QI Pilot Project Resources 1) Hereditary Cancer Resource Folder – Sample Documents Outline HBC QI Data Collection
This project is supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) through the National Association of Chronic Disease Directors (NACDD) |